Muscle Rigidity in Parkinson’s

Rigidity, or the stiffness and inflexibility of the limbs, neck or trunk, is one of the primary motor symptoms of Parkinson’s. However, not all patients with Parkinson’sexperience rigidity. In Parkinson’s, rigidity can prevent you from moving easily, and this lack of easy movement can cause discomfort or pain in the muscles.
The other main primary motor symptoms are tremor, particularly when the limb is at rest, postural instability, impaired balance or difficulty standing or walking, and bradykinesia (the gradual loss and slowing down of spontaneous movement).
Muscles usually stretch when they move and relax when they are at rest, and rigidity causes the muscles to remain stiff and unable to rest. When your muscles are rigid and you’re having trouble moving them, this can leads to several other problems.
When coupled with bradykinesia, rigidity may cause a person with Parkinson’s:
– Not to be able to move or extend their arms or legs very far, which means they take shorter steps and may not swing their arms as they walk. This can lead to problems with balance and could increase risk of falls.
– to have problems carrying out day to day tasks that require small, careful movements such as buttoning a shirt or tying up shoe laces.
– to have trouble with normal facial expressions, leading to a mask-like blank expression(Hypomimia). Rigidity can interfere with normal communication both by the masked face appearance leaving others uncertain of your emotional reaction to the conversation and by changing the appearance of your written words as well. This expression can, in turn, affect your relationships, as your facial expression may suggest that you feel differently about a situation based on body language.
If your face is rigid and mask-like, a speech therapist may be able to help you exercise those muscles and keep them more flexible. It’s best to start this type of therapy soon after your diagnosis to have the most success with it.
When moving one side of the body, rigidity can worsen the movement on the opposite side of the body. For example, stiffness in your left arm and shoulder may be enhanced when you use your right arm.
The muscle rigidity in Parkinson’s disease can impact every area of your life including walking, eating and mobilising around the home for example getting out of a chair or turning in bed.
Stress, anxiety and depression can all worsen motor-symptoms and make rigidity worse. If you suffer from any of these, treating this can ultimately improve rigidity and even tremor.
The muscle rigidity in Parkinson’s Disease can impact every area of your life. Going through a normal day, rigidity affects mobility by making it difficult walking, turning, with the stopped posture disrupting the normal way in which landmarks are used to navigate safely. Eating can be affected, and even getting out of a chair or turning in bed can be difficult.

Treatment
Thankfully, treatment and therapies can improve the quality of life for people with Parkinson’s. It includes educating family and friends about Parkinson’s disease along the spectrum from the difficulty in interpreting facial expressions to the importance of fall prevention.
Exercise
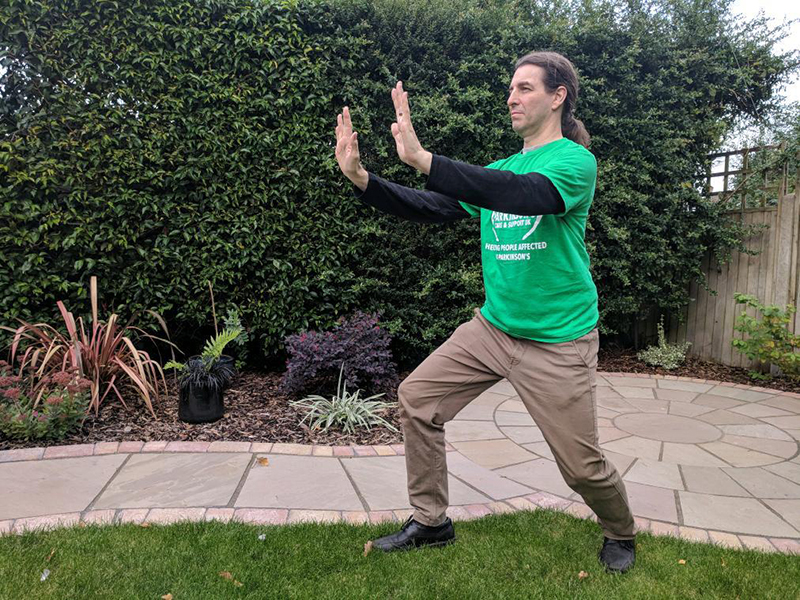
Regular exercise can keep your muscles more flexible and will keep you moving better for longer. Although it can be difficult to get motivated to exercise, especially if your muscles don’t want to cooperate. Increasing everyday movement can help improve motor symptoms, which in turn helps prevent stiff muscles. Exercises such as Yoga, Tai Chi and Qigong are really important to practice as they can improve a person’s physiological ability to move independently and safely so that they can carry out daily functional activities at home, work and in the community. They also improve balance, posture and walking. Standing yoga poses target the hip extensor, knee extensor and ankle plantar flexor, which support centre-of-mass during walking and may improve overall stability.
Balance training is an important component of any Parkinson’s therapy. Research shows Tai Chi-related improvements in balance and an associated reduction in fear of falling; this can also help keep people with Parkinson’s active in their community for longer. Join our free Parkinson’s exercise classes where you can enjoy Tai Chi, Qigong, Yoga, Boxing and more.
While any level of physical activity can be beneficial for Parkinson’s, research suggests that high-intensity interval training, or HIIT, is also more effective at improving a range of disease symptoms
A HIIT session generally involves 30 to 60 seconds of hard exercise near the top of a person’s limit, followed by an easy recovery exercise for the same amount of time. Then the process is repeated for about 20 minutes. One convenient feature of HIIT is that it can be adapted to exercises many already do, such as walking, jogging and cycling.
One study demonstrated that HIIT could alleviate the rigidity and excessive muscle tone that makes it difficult for people with Parkinson’s to move their arms and legs. The researchers, from the University School of Physical Education in Krakow, Poland, showed in 11 patients with mild to moderate Parkinson’s symptoms that eight weeks of HIIT, three times a week, on a stationary bike had a global benefit, improving both lower and upper body function.
Physiotherapy
Working with a physical therapist can be very helpful in designing a routine, as well as to learn more about how to improve your mobility, balance and reduce your risk of falls. Physical therapists can help you optimise your exercise routine, re-learn challenging tasks or stay safe and independent in the home. Some of the most common movement goals for people with Parkinson’s include:
- Learning about exercises
- Improving walking, balance or posture
- Addressing fall risk
- Treating pain
Some drugs prescribed for Parkinson’s disease can help to reduce rigidity with the consequences of side effects.
All prescribed medications can have potential side effects. This is no different to medications used to treat Parkinson’s. In fact, many people are unable to differentiate the difference between the symptoms of Parkinson’s and the effects of medication, commonly blaming Parkinson’s for how they are feeling. The side effects of medication can have a big impact on people’s lives and many battle keeping these under control along with Parkinson’s symptoms.
Tips
The following suggestions may help:
- Continue your normal routine and daily activities as long as you are able.
- Follow a simple exercise programme to keep your muscles flexible and strong.
- Adjust your routine so that you do things that might tire your muscles when you feel least stiff.
- Remove or firmly secure loose rugs that you can trip over and rearrange furniture to make it easier to move around at home.
- If it does take you longer to perform tasks, allow yourself extra time to do them. This will help you to remain calm and minimise stress. Stress can make rigidity worse!
- Maintain a positive attitude – this can help with all sorts of difficulties.




